Research selection
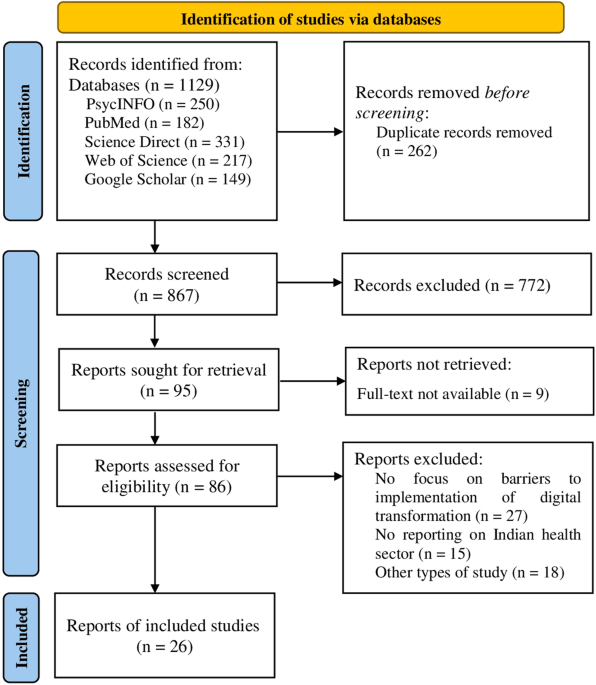
The search of electronic databases returned a total of 1,129 articles. Of these, 250 were from PsycINFO, 182 from PubMed, 331 from Science Direct, 217 from Web of Science, and 149 from Google Scholar. The PRISMA flow diagram depicts the complete search process for this systematic review (Figure 1). After deduplication, the titles and abstracts of 867 records were screened according to inclusion and exclusion criteria. Title and abstract screening subsequently removed 772 studies. Nine of the 95 records searched could not be retrieved because the full text was not accessible. Therefore, 86 reports were evaluated for inclusion and 60 studies were removed as they did not meet the eligibility criteria (not focused on barriers to implementation of digital transformation in the healthcare sector) (n = 27), conference proceedings and review papers (n = 18), and no focus on Indian health (n = 15)). Therefore, the final synthesis includes 26 studies highlighting the barriers to implementing various digital technologies in the healthcare sector.
Figure 1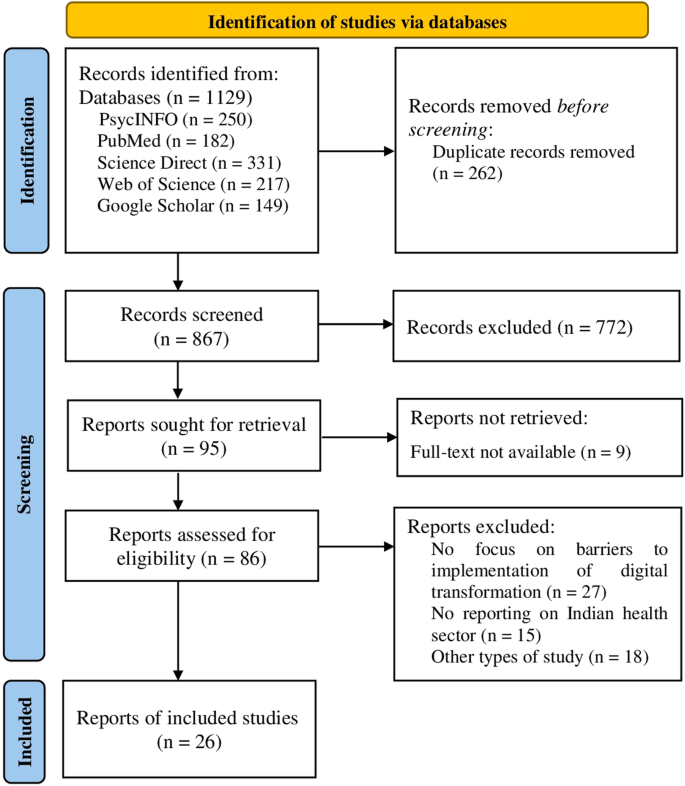
PRISMA flowchart for this systematic review.
Research characteristics
The final sample for the present review included 26 studies conducted across India from 2017 to 2022 (Table 1). Two studies were published in 2022 (Prakash and Das, 2022; Sampathkumar et al., 2022) and 16 studies were published in 2021 (Birapareddy et al., 2021; Banerjee et al., 2021; D' Souza et al., 2021; Garg et al., 2021) Ghoshal et al., 2021; Mathew et al., 2021; Naveen et al., 2021. ., 2021; Sandhu et al., 2021; Shambu et al., 2021; Ullas et al., 2020 (Biswas et al., 2020);Pandey et al., 2020;Puliyath et al., 2021;Thenral and Annamalai , 2021), two in 2018 (Bhatt et al., 2018), and two in 2017 (Mohan et al., 2018), 2017; Powell et al., 2017). The included studies consisted of quantitative/cross-sectional studies (n = 10) (Bairapareddy et al., 2021; Sinha Deb et al., 2018; Ghoshal et al., 2021; Kumar et al., 2021; Mohan et al., 2017; Nair et al., 2021; Pandey et al., 2021; Ullas et al., 2021), quantitative/cohort studies (Biswas et al., 2021), D'Souza et al. ., 2021, Garg et al., 2021; Sandhu et al., 2021. et al., 2021), qualitative research (n = 5) (Banerjee et al., 2021; Bhatt et al., 2018; Menon et al., 2021; Faujdar et al., 2021; thenral and Annamalai, 2021) , and mixed methods studies (n = 3) (Mathew et al., 2021; Prakash and Das, 2022; Sampathkumar et al., 2022). Participants included the general population, women who have given birth, medical professionals, patients and caregivers, academic experts, smartphone users, and technology experts. The current findings provide a comprehensive understanding of the barriers to the adoption of digital transformation in the Indian healthcare sector.
Table 1 Summary of study characteristics.
Risk of bias in research
The risk of bias in quantitative cross-sectional studies (n = 10) and qualitative studies (n = 5) was low, whereas the risk of bias in cohort studies was generally low to moderate (see supplementary information). Detailed results of the quality assessment of the mixed methods study (n = 3) are provided in the Supplementary Table (see Supplementary Table 4). Additionally, no studies were excluded based on the level of quality assessment.
Barriers to implementing digital transformation in healthcare
Several previous studies have identified potential barriers to implementing digital transformation in India. For a successful digital health transformation, it is necessary to identify national barriers to digital health transformation. As a result, the findings were consolidated into the following themes: lack of network coverage and information technology (IT) infrastructure, high installation and operational costs, lack of medical records and specialists, lack of physical exams, and lack of data. These include accuracy and misdiagnosis, data privacy confidentiality, language and communication barriers, user barriers, and ethical, legal, and accountability issues.
Lack of network coverage and IT infrastructure
Weak network coverage (Banerjee et al., 2021; Desingh and Baskaran, 2021; Menon et al., 2021; Puliyath et al., 2020; Raheja et al., 2021; Sampathkumar et al., 2022; Sandhu et al. ., 2021; Ullas et al., 2021), and lack of IT infrastructure (Desingh and Baskaran, 2021) has been described as a major barrier to digital transformation in the healthcare sector. In this context, lack of basic technological infrastructure such as smartphones is a potential barrier to implementing digital health in India (Kumar et al., 2021; Puliyath et al., 2020 ; Sandhu et al., 2021). In this context, patients were required to participate in telemedicine using their family members' smartphones (Garg et al., 2021).
High installation and operating costs
Financial concerns have been identified as a barrier to the implementation and adoption of digital transformation in the healthcare sector (Birapareddy et al., 2021; Bhatt et al., 2018). A study by Powell et al., (2017) found that hospitals implementing EHR systems were concerned about the funding required to purchase and implement EHRs, the ongoing costs of maintaining EHR systems, and concerns about the ambiguity of EHR systems. It became clear that they were aware of several barriers to adoption, including: return on investment (ROI) from EHRs (Powell et al., 2017); In this context, the lack of repair facilities at the installation site is also a major barrier (Menon et al., 2021). However, qualitative interviews in one study revealed that the high cost of smart devices is a barrier to using mobile-based apps for healthcare (Sinha Deb et al., 2018 ).
Lack of medical records and specialists
Digital health is a new platform that is being developed recently in India. Rapid implementation of digital transformation can lead to difficulties in obtaining domestic EHRs (Menon et al., 2021; Puliyath et al., 2020) and experts (Bairpareddy et al., 2021) . According to one study, the main difficulty for clinicians in using telemedicine is a lack of operational technical expertise (Sandhu et al., 2021). Similarly, in another study, 53% of healthcare professionals identified lack of expertise as the main barrier to effective implementation of a smartphone-based telerehabilitation program for patients with chronic obstructive pulmonary disease ( Bairapareddy et al., 2021).
lack of physical examination
One of the major barriers to the acceptance of digital health is the lack of a physical exam, which is a necessary prerequisite for an effective doctor-patient relationship (Kumar et al., 2021; Mathew et al., 2021; Puliyath et al., 2020; Raheja et al., 2021; Ullas et al., 2021). Furthermore, patients expressed dissatisfaction with the rapport established after face-to-face consultations (Garg et al., 2021). Similarly, in a study by D'Souza et al. (2021), older patients preferred face-to-face consultations. This flaw in digital transformation could be addressed by referring patients whose symptoms or reports require medical examination to nearby medical centers (Kumar et al., 2021).
Data accuracy and misdiagnosis
Another potential barrier to successful adoption of digital health practices is the accuracy of data transmission. In a study by Raheja et al. (2021), 6% of participants faced difficulties during telephone consultations due to misunderstanding of prescriptions by patients or pharmacists. Similarly, limited connectivity (Banerjee et al., 2021) and unfamiliar technology (Sinha Deb et al., 2018; Ghoshal et al., 2021; Sandhu et al., 2021) make it difficult for patients to It was difficult to understand medical advice and medicines. , 2021; Ullas et al., 2021), illiteracy (D'Souza et al., 2021; Kumar et al., 2021; Naveen et al., 2021), and lack of clarity in advice given by clinicians (Sandhu et al. ., 2021) ., 2021).
Data privacy and confidentiality
Compared to in-person consultations, digital health is more vulnerable to security and privacy risks. In digital health systems, data protection is threatened by leakage of sensitive information and data sharing with third-party apps (Biswas et al., 2020; Menon et al., 2021). The healthcare industry is one of the most critical sectors due to the need to protect highly sensitive patient data, so data security and confidentiality concerns are critical to implementing digital health transformation. (Desingh and Baskaran, 2021; Powell et al. , 2017; Purakash and Das, 2022; Thenral and Annamalai, 2021).
language and communication barriers
Effective communication between patients and healthcare providers is essential and often leads to digital health success. This is certainly a challenge in implementing digital transformation in the healthcare sector (Menon et al., 2021; Mathew et al., 2021; Naveen et al., 2021; Raheja et al., 2021). Language is one of the key issues in digital transformation (Sinha Deb et al., 2018; Mohan et al., 2017; Naveen et al., 2021; Sandhu et al., 2021). In their study, Satgunam et al. (2021) reported that although most respondents felt comfortable downloading and using a telephone consultation app, patients who do not understand English may face some difficulty navigating the application. Masu. Furthermore, Pandey et al. (2020) reported that insufficient communication methods on the part of patients may be a reason for the decline in telemedicine. In this context, another study was also reported by Kumar et al. (2021) showed that the unavailability of an appropriate environment for communication is a major barrier to incorporating teleconsultation into practice. Of note, two studies reported that video-based teleconsultation was the most preferred communication method for patients (Raheja et al., 2021; Nair et al., 2021).
Barriers to use
Several user challenges in digital health are barriers to implementing digital transformation in the healthcare industry. Findings show that difficulties in making regular doctor's appointments and getting medicines on time (Ullas et al., 2021) and long distance travel for laboratory tests and report uploads (at least in 2021) The study highlights a variety of barriers to the use of telemedicine, including: – Personal consultation before moving to digital mode (Shambu et al., 2021), dependence on computers and digital technicians (Faujdar et al., 2021), lack of on-site repair equipment (Menon et al., (2021) and improving availability of challenged medicines (Kumar et al., 2021).
Ethical, legal and accountability concerns
A common reason for not using digital consultation was fear of possible legal repercussions. There is a risk of misdiagnosis while conducting telemedicine, which can have serious medical consequences (Pandey et al., 2020). In this context, a study by Thenral and Annamalai (2021) found that almost all respondents cited issues related to ethical, legal, and accountability implications as challenges to digital consultations. Furthermore, another study reported that increased transparency in the implementation of digital health systems made healthcare workers feel anxious as they increased work stress and had to be more careful with data entry. (Faujdar et al., 2021).