Vakulin, A. et al. Individual differences and predictors of driving simulator impairment in patients with obstructive sleep apnea syndrome. J. Clin. Sleep Med. 10, 647–655 (2014).
George, CFP Sleep apnea, wakefulness, car accident. morning. J. Respier. critical. Care Med. 176, 954–956 (2007).
Alhejaili, F. et al. Prevalence of obstructive sleep apnea syndrome in Saudi Arabian pilots. nut. Science. Sleep 13, 537–545 (2021).
Gurubhagavatula, I., Tan, M., and Jobanputra, AM OSA professional transportation operations: safety, regulation, and economic implications. Chest 158, 2172–2183 (2020).
Chapman, J., Naweed, A., Wilson, C. & Dorrian, J. Sleep for heart health: investigating the relationship between workday sleep, holiday sleep and cardiovascular risk among Australian train drivers. Ind. Health 57, 691–700 (2019).
Filtness, AJ & Naweed, A. Causes, consequences and countermeasures for driver fatigue in the railway industry: A train driver's perspective. Applied ergon. 60, 12–21 (2017).
Dorrian, J., Chapman, J., Bowditch, L., Balfe, N., Naweed, A. A study of schedules, sleep, health status and driving performance of train drivers in Australia and New Zealand. Science. Rep. No. 12, 1–11 (2022).
Abeyaratne, M., Casolin, A. & Luscombe, G. Safety accidents and obstructive sleep apnea syndrome among railway workers. Occupy. medicine. 73(2), 97–102 (2023).
Hocking, B. The Waterfall Train Accident Study: Implications for Medical Examinations of Safety-Critical Workers. medicine. J. Aust. 184, 126–128 (2006).
National Transportation Commission. National standards for health assessment of railway safety workers. (2017).
MW Johns A new way to measure daytime sleepiness, the Epworth Sleepiness Scale. Sleep 14, 540–545 (1991).
Babor, TF, Higgins-Biddle, JC, Saunders, JB, Monteiro, MG Audit. Alcohol Use Disorders Identification Test (AUDIT): Guidelines for use in primary care (2001).
Kessler, RC et al. Short-term screening monitors population prevalence and trends in nonspecific psychological distress. Psychol. medicine. 32, 959–976 (2002).
Mina, R. & Kassoline, A. National standards for Australian railway workers established after five years. Occupy. medicine. 62, 642–647 (2012).
Mina, R. & Kasolin, A. National standards for railway safety worker health assessment: First year. medicine. J. Aust. 187, 394–397 (2007).
Naweed, A., Chapman, J. & Trigg, J. Tell them what they want to hear and get back to work: Insights into the usefulness of current occupational health assessments from the perspective of train drivers. Transparent Resolution Part A: Policy Practice. 118, 234–244 (2018).
Google Scholar
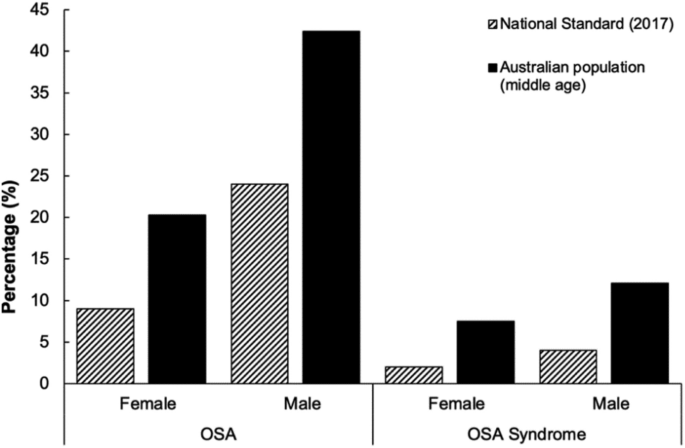
Colquhoun, CP & Casolin, A. The impact of railroad medical standards on the prevalence of obstructive sleep apnea syndrome. Occupy. medicine. 66, 62–68 (2016).
McArdle, N. et al. Prevalence of common sleep disorders in a middle-aged community sample. J. Clin. Sleep Med. 18, 1503–1514 (2022).
New Mexico, Punjab, et al. Sleep-disordered breathing, glucose intolerance, and insulin resistance: A study of heart health during sleep. morning. J. Epidemiol. 160, 521–530 (2004).
Lechat, B. et al. Large nocturnal fluctuations in sleep apnea severity are associated with uncontrolled hypertension. NPJ digit. medicine. 6, 57 (2023).
Nieto, F.J. Associations between sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Survey. JAMA 283, 1829–1836 (2000).
Gottlieb, DJ et al. A prospective study of obstructive sleep apnea and coronary heart disease and heart failure: The Sleep Heart Health Study. Circular 122, 352–360 (2010).
Hsieh, H.-F. & Shannon, S.E. Three approaches to qualitative content analysis. quality. Health Research Institute 15, 1277–1288 (2005).
Naweed, A., Bowditch, L., Chapman, J., Dorian, J., Balfe, N. How are you doing? The analysis of the railway signals passed in the hazard proforma and the extent to which they capture the system influences subsequent accidents. Saf. Science. 151, 105726 (2022).
R core team. RStudio: Integrated development environment for R v3.6.2. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.r-project.org/ (2019).
Mathew, J. & Benekohal, RF Prediction of highway and railroad grade crossing accidents using zero-inflated negative binomial and empirical Bayes methods. J. Safety Research Institute 79, 211–236 (2021).
Jilotek, MR and Turner, JR Why it is nonsense to use retrospective power analysis to conduct post-hoc analyzes of studies. J. Clin. High blood pressure. 20, 408–410 (2018).
Australian Railway Association. Workforce Development Report – Railroad Workforce Data 2014 (2014).
Nagappa, M. et al. Validation of the STOP-bang questionnaire as a screening tool for obstructive sleep apnea among different populations: A systematic review and meta-analysis. PLoS One 10, e0143697 (2015).
de Menezes-Júnior, LAA et al. Predictive value of BOAH and apnea score for screening obstructive sleep apnea syndrome in shift drivers. Sleep Med X 6, 100084 (2023).
de Menezes Júnior, LAA Diagnostic accuracy of the Berlin Questionnaire and NoSAS score in detecting the risk of obstructive sleep apnea syndrome in other shift workers. sleep breathing. 26, 743–751 (2022).
Senator McKay Fatal Consequences: Obstructive Sleep Apnea in Railway Engineers. Ann. Fam. medicine. 13, 583–586 (2015).
Reynolds, A.C. et al. Sickness absenteeism is associated with sleep problems independent of sleep disorders: Results from the 2016 Sleep Health Foundation National Survey. Sleep Health 3, 357–361 (2017).
Bjornsdottir, E. et al. Quality of life in untreated sleep apnea patients compared with the general population and changes after treatment with positive airway pressure. J. Sleep resistance. 24, 328–338 (2015).
Edwards, C., Almeida, OP & Ford, AH Obstructive sleep apnea and depression: A systematic review and meta-analysis. Maturitas 142, 45–54 (2020).
Azarbarudin, A. et al. Hypoxic stress due to sleep apnea predicts cardiovascular disease-related mortality: a study of osteoporotic fractures and a study of cardiac health during sleep in men. EUR. Heart J. 40, 1149–1157 (2019).
Azarbarudin, A. et al. Sleep apnea-specific hypoxic stress predicts the development of heart failure. Chest 158, 739–750 (2020).
Lechat, B. et al. A new approach to better define sleep disorders and their effects. front. Neuroscience. 15, 751730 (2021).
Lechat, B. et al. A new brainwave-derived measure of disrupted delta wave activity during sleep predicts all-cause mortality risk. Ann. morning. Chest. Society 19, 649–658 (2022).
Azarbarzin, A. et al. Sleep apnea-specific pulse rate responses predict cardiovascular morbidity and mortality. morning. J. Respier. critical. Care Med. 203, 1546–1555 (2021).
Solelhac, G. et al. Pulse wave amplitude reduction index: a biomarker of cardiovascular risk in obstructive sleep apnea syndrome. morning. J. Respier. critical. Care Med. https://doi.org/10.1164/rccm.202206-1223OC (2023).
Lechat, B. et al. Multi-night prevalence, variability, and diagnostic misclassification of obstructive sleep apnea syndrome. morning. J. Respier. critical. Care Med. https://doi.org/10.1164/rccm.202107-1761OC (2021).
Punjabi, NM, Patil, S., Crainiceanu, C. & Aurora, RN Variability and misclassification of sleep apnea severity based on multi-night testing. Chest 158, 365–373 (2020).
Lechat, B. et al. Overnight diagnosis of sleep apnea contributes to inconsistent cardiovascular outcome findings. Chest https://doi.org/10.1016/j.chest.2023.01.027 (2023).
Paciorek, M. et al. Obstructive sleep apnea syndrome in shift workers. Sleep Med. 12, 274–277 (2011).