Neurodevelopmental disorders. Diagnostic and Statistical Manual of Mental Disorders. https://doi.org/10.1176/appi.books.9780890425787.x01_Neurodevelopmental_Disorders (2024).
Straub, L. et al. “Neurodevelopmental disorders among publicly and privately insured children in the United States.” JAMA Psychiatr. 79, 232–242 (2022).
Prasad, AN & Corbett, BA. Neurodevelopmental disorders in Canadian children: Prevalence data from the National Longitudinal Survey of Children and Adolescents. J. Pediatr. Neurol. 19, 153–160 (2019).
Google Academic
Ouellette-Kuntz, H. et al. Status report of the National Epidemiological Database for Autism Research in Canada (Nedsac). Chronic Dis. Inj. Can. 32, 84–89 (2012).
Raouafi, S., Achiche, S., Raison, M. Socioeconomic disparities and difficulties accessing health services among Canadian children with neurodevelopmental disorders and disabilities. Epidemiology. Health 40, e2018010 (2018).
Anderson, LM et al. Effectiveness of early childhood development programs. A systematic review. Am. J. Prev. Med 24, 32–46 (2003).
Conti, G., Heckman, J. & Pinto, R. The impact of two high-impact early childhood interventions on health and healthy behaviors. Econ. J. (Lond.) 126, F28–f65 (2016).
Kaaresen, PI, Rønning, JA, Ulvund, SE & Dahl, LB. A randomized controlled trial of the effectiveness of an early intervention program to reduce parenting stress after preterm birth. Pediatrics 118, e9–e19 (2006).
Wojcik, MH, Stewart, JE, Waisbren, SE & Litt, JS Developmental support for infants with genetic disorders. Pediatrics 145, e20190629 (2020).
World Health Organization. World Report on Disability (Geneva, 2011).
Blauw-Hospers, CH & Hadders-Algra, M. A systematic review of the effects of early interventions on motor development. Dev. Med Child Neurol. 47, 421–432 (2005).
Clark, BG et al. Screening for language delay after critical care in term infants. Cardiol. Young. 26, 1343–1351 (2016).
Primary and Integrated Healthcare Innovation Network. COVID-19 Primary Care Rapid Clinician Survey: Summary of the third pan-Canadian survey of frontline primary care clinicians' experiences with COVID-19 (University of Michigan, accessed April 24-27, 2020).
Julien, D., Marie-Annick Le, P., Isabelle, P.-B. Early impact of the Covid-19 pandemic on face-to-face use of outpatient care: a rapid review. BMJ Open 12, e056086 (2022).
The Larry Green Centre and Primary Care Collaborative. Covid-19 Collection: Primary Care Covid-19 Survey. (Leawood, 2022).
Barney, A., Buckelew, S., Mesheriakova, V. & Raymond-Flesch, M. The Covid-19 pandemic and the rapid adoption of telehealth for adolescents and young adults: challenges and opportunities for innovation. J. Adolesc. Health 67, 164–171 (2020).
Webster, P. “Virtual Healthcare in the Age of Covid-19.” The Lancet 395, 1180-1181 (2020).
Wood, SM et al. Outcomes of rapid expansion of adolescent telehealth during the Covid-19 pandemic. J. Adolesc. Health 67, 172–178 (2020).
Ministry of Health. Bulletin 4745—Changes to the Physician Services Benefits Schedule (Schedule) in Response to the COVID-19 Pandemic, effective March 14, 2020, https://www.ontario.ca/document/ohip-infobulletins-2020/bulletin-4745-changes-schedule-benefits-physician-services (2020).
Saunders, NR et al. Physician-provided mental health care service utilization among children and adolescents in Ontario, Canada, before and during the COVID-19 pandemic. JAMA Pediatr. 176, e216298–e216298 (2022).
Autism Society of Ontario. Priority #2: Long Waitlists https://www.autismontario.com/news/priority-2-long-waitlists#:~:text=In%20March%202020%2C%20the%20Ontario,or%20youth%20aged%206%20%E2%80%93%2017 (2020).
Barua, M. et al., “Mental health ecology and urban well-being,” Health Place 69, 102577 (2021).
Moynihan, R. et al., “The impact of the COVID-19 pandemic on health service utilization: a systematic review,” BMJ Open 11, e045343 (2021).
Hessami, K. et al. The Covid-19 pandemic and infant neurodevelopmental disorders: a systematic review and meta-analysis. JAMA Netw. Open 5, e2238941 (2022).
ICES. Ices https://www.ices.on.ca/ (2024).
Schull, MJ et al. “Ice: Data, Discovery, and Better Health.” Int J. Popul. Data Sci. 4, 1135 (2020).
Benchimol, EI et al. Reporting of studies conducted using observationally routinely collected health data (records) statements. PLoS Med. 12, e1001885 (2015).
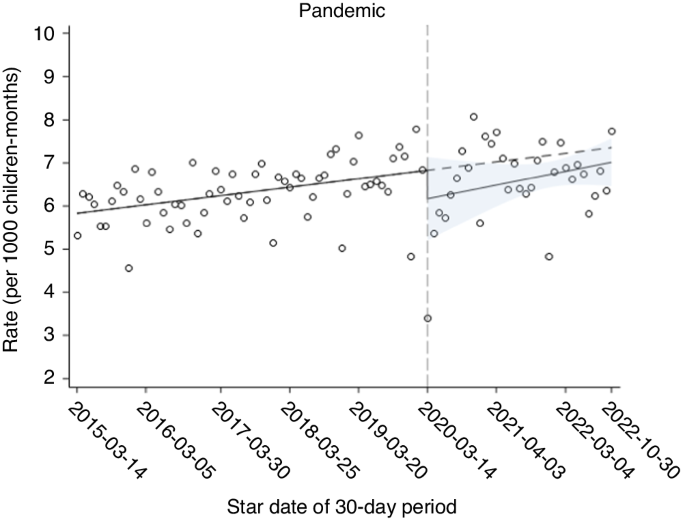
Wagner, AK, Soumerai, SB, Zhang, F. & Ross-Degnan, D. Segmental regression analysis of interrupted time series studies in drug use research. J. Clin. Pharm. Ther. 27, 299–309 (2002).
Huitema, BE & Mckean, JW Design specification issues in time series intervention models. Educ. Psychol. Meas. 60, 38–58 (2000).
Stata statistical software: Release 15 (StataCorp LLC, 2017).
Evensen, M. et al. The impact of the Covid-19 pandemic on mental health care consultations for children and adolescents in Norway: a national register study. Eur. Child Adolesc. Psychiatry 32, 1025–1035 (2023).
Koonin, LM et al., “Trends in telehealth use during the COVID-19 pandemic – United States, January-March 2020.” MMWR Morb. Mortal. Wkly Rep. 69, 1595–1599 (2020).
Ontario Ministry of Health and Long-Term Care. Changes to the Physician Services Benefit Schedule (Schedule) in Response to the COVID-19 Pandemic (effective 2020).
O'Hara, VM, Johnston, SV & Browne, NT Pediatric weight management outpatient consultations via telehealth: from pre- to post-COVID-19 pandemic. Pediatr. Obes. 15, e12694 (2020).
Canadian Institute for Health Information. Expanding Virtual Care in Canada: New Data and Information (Canadian Institute for Health Information, 2023).
Curfman, A. et al. Pediatric telemedicine in the era of the Covid-19 pandemic and beyond. Pediatrics 148, e2020047795 (2021).
Reisinger, DL et al. Provider and caregiver satisfaction with telehealth evaluations for autism spectrum disorder in young children during the Covid-19 pandemic. J. Autism Dev. Disord. 52, 5099–5113 (2022).
Virtual Care Task Force. Virtual Care in Canada: Progress and Opportunities (Canadian Medical Association, 2022).
Sheperd, L. Ontario doctors report vast majority of patient visits are in person https://www.oma.org/newsroom/news/2023/august/ontario-doctors-report-vast-majority-of-patient-visits-are-in-person/ (2023).
Saunders, N. et al. Pediatric primary care in Ontario and Manitoba following the onset of the COVID-19 pandemic: a population-based study. CMAJ Open 9, E1149 (2021).
Bhat, A. Analysis of the Spark Study Covid-19 Parent Survey: Early impacts of the pandemic on access to services, child/parent mental health, and benefits of online services. Autism Research. 14, 2454–2470 (2021).
Goodwin Cartwright, BM et al. A time series analysis of pediatric initial language delay from 2018 to 2022. JAMA Pediatr. 178, 193–195 (2024).
Charney, SA, Camarata, SM & Chern, A. Potential impact of the Covid-19 pandemic on children's communication and language skills. Otolaryngology Head and Neck Surgery 165, 1–2 (2021).
Creswell, C. et al. Young people's mental health during the Covid-19 pandemic. Lancet Child Adolesc. Health 5, 535–537 (2021).
Mete Yesil, A., Sencan, B., Omercioglu, E. & Ozmert, E. N. “Impact of the COVID-19 pandemic on children with special needs: a descriptive study.” Clin. Pediatr. 61, 141–149 (2022).
Mulkey, SB, Bearer, CF & Molloy, EJ. “Indirect effects of the COVID-19 pandemic on children are related to children's age and experience.” Pediatr. Res. 94, 1586–1587 (2023).
Zhao, Y., Luo, Y., Zhang, R. & Zheng, X. The impact of the Covid-19 pandemic on emotional and behavioral problems in children aged 1-6 years with autism spectrum disorder and developmental delay in China. Front. Psychiatry 14, 1134396 (2023).
Edlow, AG et al. Gender-specific neurodevelopmental outcomes in children born to mothers infected with SARS-Cov-2 during pregnancy. JAMA Netw. Open 6, e234415–e234415 (2023).