In a study recently published in the journal Psychiatric Research, a group of researchers evaluated the metabolic and mental health effects of a ketogenic diet (KD) in patients with schizophrenia or bipolar disorder who already had metabolic abnormalities.
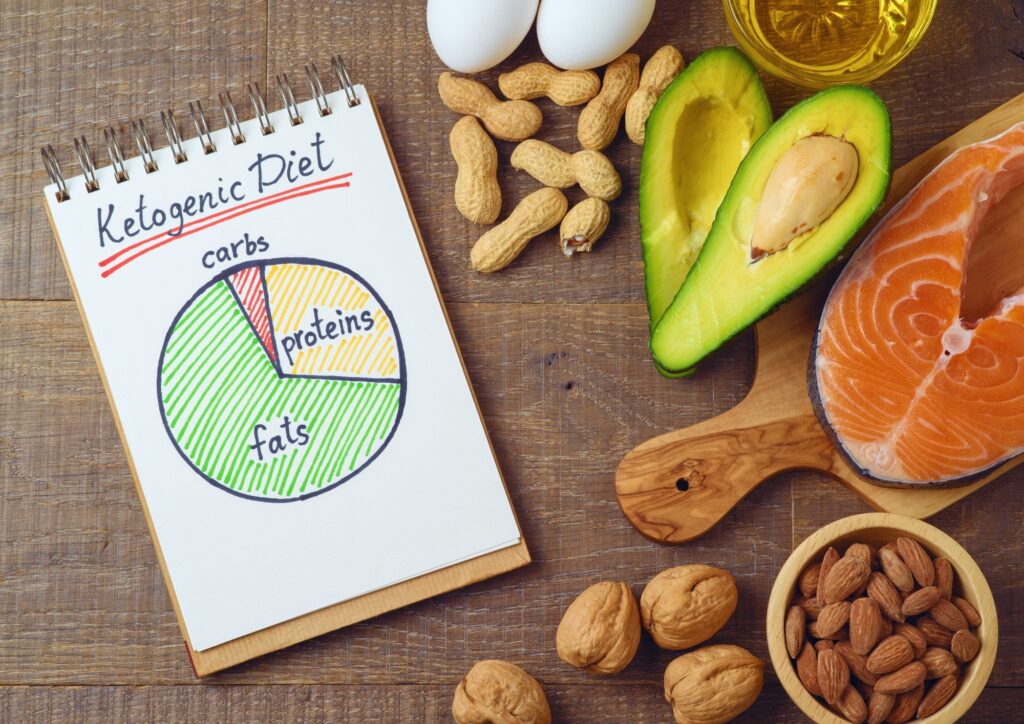
 Study: Ketogenic diet intervention on metabolic and mental health in bipolar disorder and schizophrenia: a pilot trial. Image credit: Maglara/Shutterstock
Study: Ketogenic diet intervention on metabolic and mental health in bipolar disorder and schizophrenia: a pilot trial. Image credit: Maglara/Shutterstock
background
Millions of people worldwide suffer from severe mental illnesses, such as schizophrenia (24 million) and bipolar disorder (50 million). Current treatments often lead to resistance and metabolic side effects, causing non-adherence. Traditional neuroleptics may reduce life expectancy while benefiting long-term mortality in schizophrenia. KDs, effective in treating epilepsy, provide the brain with an alternative fuel source and reduce neuronal excitability and inflammation. Emerging evidence suggests that metabolic dysfunction underlies psychiatric illness. Patients with severe mental illness are at high risk for metabolic syndrome, so further research into the potential of KDs to improve metabolic and psychiatric outcomes is essential.
About the Research
The study enrolled 23 participants aged 18-75 years who were taking psychotropic medications and met criteria for being overweight or metabolically abnormal. Twenty-one participants completed the study (5 with schizophrenia and 16 with bipolar disorder). Eligibility was determined by a comprehensive assessment and clinical examination. Participants received educational materials, a cookbook, resources, and a personal coach.
The prescribed KD consisted of 10% carbohydrate, 30% protein, and 60% fat, with a goal of achieving blood ketone concentrations of 0.5–5 mM. Compliance was monitored based on ketosis levels. Blood samples were analyzed for metabolic markers, and vital signs, body composition, and psychiatric assessments were recorded at baseline, 2 months, and 4 months. Remote participants self-reported data and attended local facilities for evaluation. The study also evaluated potential side effects of the KD compared to psychiatric medications and was approved by the Stanford University Institutional Review Board and registered at ClinicalTrials.gov (NCT03935854).
Statistical analysis was performed using standard methods in Microsoft Excel and data were recorded in Research Electronic Data Capture (REdCap). Baseline and final measurements were compared with paired t-tests and nominal data were assessed with McNemar's test and chi-square analysis. Due to the exploratory nature of this study, significance testing was not performed, but a p-value <0.05 was considered significant. The analysis included percent changes in metabolic and psychiatric outcomes and provides insight into the potential benefits of a KD for people with severe mental illness.
research result
The data analysis cohort included 23 participants, including 5 with schizophrenia and 16 with bipolar disorder. Fourteen participants were fully compliant with the KD, 6 were semi-compliant, and 1 was non-compliant.
Initially, 29% of participants met criteria for metabolic syndrome. By the end of the study, none met these criteria (p < 0.05). Primary metabolic outcomes included a 10% reduction in mean body weight (p < 0.001), an 11% reduction in waist circumference (p < 0.001), a 6.4% reduction in systolic blood pressure (p < 0.005), a 17% reduction in fat mass index (p < 0.001), and a 10% reduction in body mass index (BMI) (p < 0.001). Visceral adipose tissue was reduced by 27% (p < 0.001), high-sensitivity reactive protein (hsCRP) by 23%, triglycerides by 20% (p < 0.02), and small dense low-density lipoprotein (LDL) by 1.3%. Increases in LDL (21%) and high density lipoprotein (HDL) (2.7%) were observed. Hemoglobin A1c (HbA1c) decreased by 3.6% (p < 0.001) and homeostasis model assessment of insulin resistance (HOMA-IR) decreased by 17% (p < 0.05). There was no significant change in 10-year atherosclerotic cardiovascular disease (ASCVD) risk score in the entire cohort, but adherent participants experienced an 11% improvement (p < 0.01).
Psychiatric outcomes revealed a 31% improvement in Clinical Global Impression severity score (p < 0.001). Recovery rates increased from 33% at baseline to 75% at the end of the study, with 100% of the adherent group having recovered. Overall, 43% of participants recovered (50% adherent, 33% semi-adherent) and 79% had a notable improvement in severity (92% adherent, 50% semi-adherent). Of participants with bipolar disorder, 69% had an improvement of at least 1 point in severity, with recovery rates increasing from 38% to 81%. All adherent bipolar participants were in or recovering by the end of the study. Psychiatric improvements included a 17% increase in life satisfaction (p < 0.002), a 17% improvement in global functioning rating (p < 0.001), and a 19% improvement in sleep quality (p < 0.02). Participants with schizophrenia experienced a 32% decrease in Brief Psychiatric Rating Scale scores (p < 0.02).
Common side effects of the KD, such as headache, fatigue, and constipation, were initially noted but reduced to minimal levels after 3 weeks. Qualitative feedback from participants highlighted significant improvements in anxiety, mood stability, and overall quality of life, with some experiencing significant personal changes.
Conclusion
In summary, studies of patients with schizophrenia and bipolar disorder who received a KD alongside psychiatric medications revealed significant psychiatric and metabolic improvements. Psychiatric outcomes showed a 31% improvement in psychiatric illness severity, with 79% of symptomatic participants experiencing significant improvement, especially among adherents. Metabolic outcomes included reductions in weight, waist circumference, systolic blood pressure, body mass index, BMI, visceral adipose tissue, HbA1c, and triglycerides. Common KD side effects decreased after 3 weeks. These results suggest that the KD is a feasible and effective adjunctive treatment to improve psychiatric and metabolic health in this population.