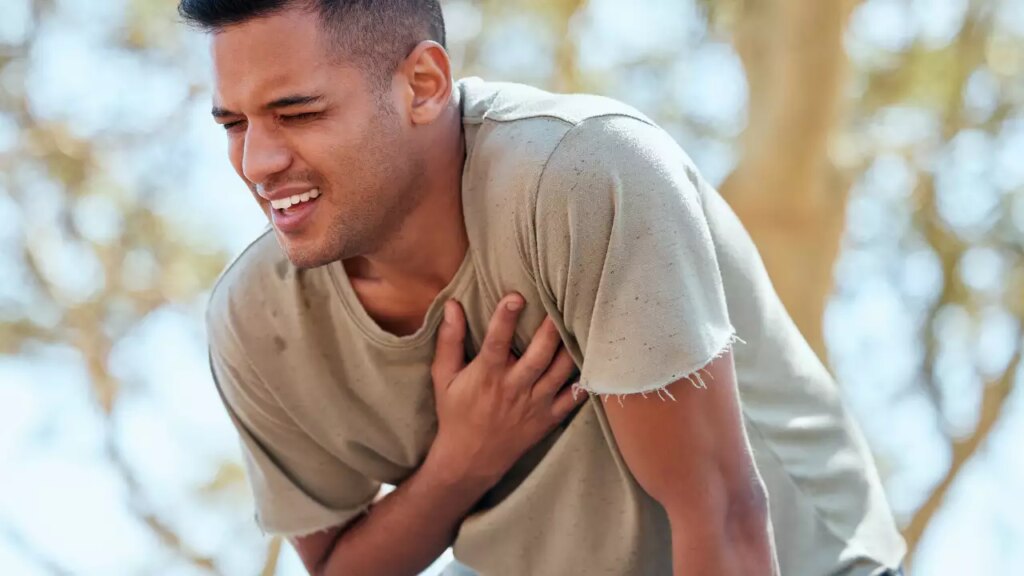
In recent years, there has been a notable increase in the incidence of heart attacks among young men aged 30-45 years, a trend that is particularly worrying when compared to women in the same age group. This alarming increase may be due to a combination of biological, lifestyle, and pandemic-related factors. Genetically, men are more susceptible to cardiovascular risk factors such as high blood pressure and high cholesterol earlier than women. Lifestyle choices such as unhealthy diet, lack of exercise, higher rates of smoking and drug use, and chronic stress due to work and economic pressures contribute significantly to this problem. Moreover, the COVID-19 pandemic exacerbates these risks by promoting sedentary behavior, increasing mental health problems, and leading to unhealthy coping mechanisms.
Historical Perspective
Historically, heart attacks have been primarily associated with men, primarily because early studies and clinical trials were conducted primarily with men. This male-centric view led to the misconception that cardiovascular disease is less of a threat to women, resulting in large gender disparities in recognition, diagnosis, and treatment. For women, heart attack symptoms are often atypical, such as nausea, fatigue, or back pain rather than the typical chest pain experienced by men. This difference in symptoms led to misdiagnosis and delayed treatment for women. Over time, increased awareness of these disparities has prompted gender-specific research and improved understanding and management of heart disease in women.
Recent trends
In recent years, heart attacks have been on the rise, especially among younger adults under the age of 35, challenging the traditional view that they primarily occur in older adults. This trend is driven by lifestyle factors such as physical inactivity and poor nutrition, as well as rising rates of obesity, diabetes, and stress. Although advances in prevention and treatment have reduced overall incidence in developed countries, socioeconomic and ethnic disparities remain, and the risk of cardiovascular disease has been further exacerbated by the COVID-19 pandemic. Addressing these issues requires increased awareness and gender-specific strategies to improve outcomes for all patients.
factor
Biological factors
One of the main biological factors is the difference in genetics and hormone composition between men and women. Men generally have higher risk factors such as high blood pressure and dyslipidemia. Elevated testosterone levels, common in men, affect cholesterol levels and blood pressure, increasing the risk of cardiovascular disease. In addition, men are more likely than women to develop conditions such as high blood pressure, diabetes, and metabolic syndrome at an earlier age, significantly increasing their risk of cardiovascular disease.
Lifestyle factors
Lifestyle choices play a major role in health disparities between young men and women. Unhealthy eating habits and higher rates of obesity are more prevalent among young men. Excessive consumption of processed foods high in fat and sugar is a major factor in cardiovascular disease risk. Furthermore, sedentary lifestyles are increasingly common, especially with the rise in remote working, and men are less likely to engage in regular exercise.
Smoking and alcohol consumption are additional lifestyle factors that disproportionately affect men. Men are more likely to smoke and consume excessive alcohol, both of which are established risk factors for heart disease. Additionally, men are often less likely to seek help for mental health issues, leading to unmanaged stress, anxiety and depression. Chronic stress, in particular, can be a significant contributor to high blood pressure and other cardiovascular risks.
Post-COVID factors
The COVID-19 pandemic has introduced new factors that may worsen the risk of heart attack in young men. The virus itself affects the heart and blood vessels and has been associated with increased cardiovascular risk. Young men in particular may be experiencing more severe symptoms and complications that lead to heart problems.
During the pandemic, access to healthcare has been significantly hindered, with many routine medical visits and preventive care appointments postponed or skipped. Because men are less likely to seek routine healthcare in the first place, they may have missed important early interventions for cardiac disease during this time. Additionally, there have been rare reports of myocarditis (inflammation of the heart muscle) following mRNA COVID-19 vaccination, which appears to be more prevalent in younger men and may contribute to the increased incidence of cardiac-related problems.
The pandemic has also led to major lifestyle changes, including increased sedentary behaviour, unhealthy eating habits and elevated stress levels – changes that can significantly increase the risk of cardiovascular disease.
Comparative analysis with women
There are several reasons why younger women in the same age group do not experience an increased incidence of heart attacks: Premenopausal women benefit from the protective effects of estrogen, which can lower their risk of heart disease, an advantage that men do not have. Women are generally more proactive in seeking medical care and following health recommendations, which allows them to better manage their risk factors.
In addition, women may generally have lower rates of smoking and excessive alcohol consumption and may lead healthier lifestyles than men. Traditional gender roles also influence lifestyle choices, and men may experience different types and levels of work-related stress compared to women.
Women who experience a heart attack often are not immediately recognized as having a heart attack due to atypical symptoms, leading to misdiagnosis and delayed treatment.
Conclusion
The higher incidence of heart attacks among young men aged 30-45 years compared to women is likely due to a combination of biological predispositions, lifestyle choices, and certain pandemic-related factors. Addressing these issues through targeted public health interventions, improved access to healthcare, and lifestyle modifications is essential to alleviate this growing concern. Understanding these underlying causes can better equip young men to take control of their cardiovascular health and reduce their risk of heart disease.
(Article by Dr. Parin Sangoy, Cardiologist, Wockhardt Hospital, Central Mumbai)